Phone: 201-420-7903
Fax: 201-420-7986
Offices
Below is a listing of conditions treated and information patients may find useful when deciding on what treatment to choose
Early diagnosis of a hepatoma (also called primary liver cancer, hepatocellular cancer, or HCC) gives the best chance of long term survival. Patients needing routine liver cancer surveillance are: 1) all patients with cirrhosis, and 2) patients with hepatitis B infection and detectable virus growing in their blood. The most common causes of cirrhosis in the United States are hepatitis C and/or B infection, alcohol over use, and fatty liver. Unfortunately, 7 out of 10 patients with liver cancer have advanced cancer when found and will not benefit from surgical removal or liver transplant.
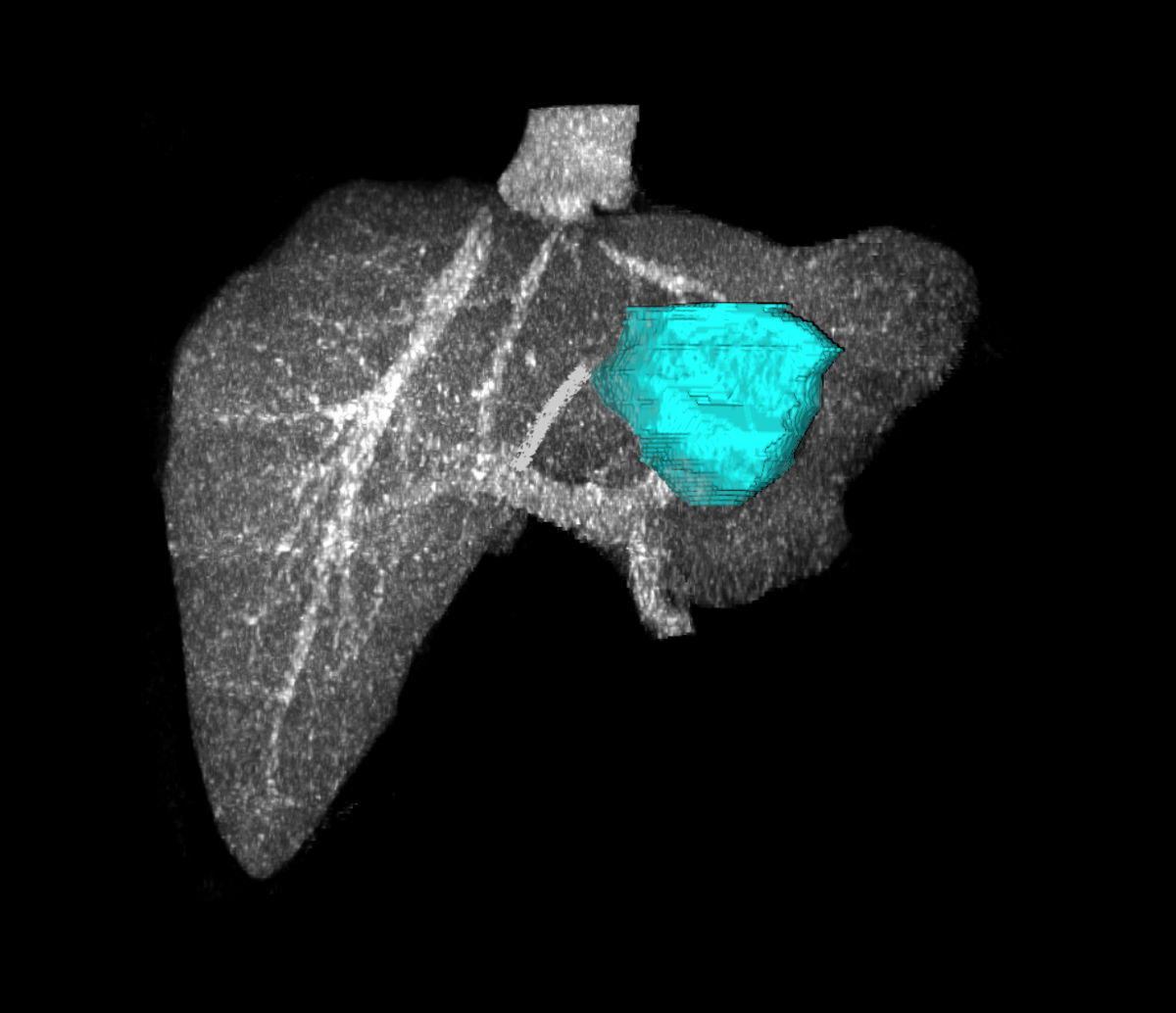
The most common cancer to the liver is metastatic from the colon or rectum. Surgical removal of cancer in the liver from the colon or rectum gives patients a 30-35% chance of being alive 5 years after surgery. Without surgery, most patients die within 12-18 months after diagnosis. Predictors of outcome include tumor size greater than 5 centimeters, having more than one tumor, having positive lymph nodes at the initial colorectal surgery, having a CEA greater than 200, and time between original colorectal surgery and development of metastatic tumor in liver less than 1 year. A patient without any of these risk factors has about a 7 out of 10 chance of being alive in 5 years. As a patient has more risk factors, their chance of surviving decreases. If a patient has all 5 risk factors, they have a 1 out of 10 chance of being alive in 5 years.
Because neuroendocrine cancers spreading to liver are usually slow growing and occur without cirrhosis of the liver, most patients are eligible for surgical removal. In patients undergoing surgery, 5 out of 10 patients will be alive 5 years following surgery. Most liver surgery for removal of a metastatic neuroendocrine cancer in the liver can be performed laparoscopically
In patients with slow growing large cancer that are not removable by surgery, liver transplant is an option. Patients can have a prior site where the cancer was removed, such as the pancreas. However to be considered a liver transplant, there can be no cancer outside the liver or invasion of cancer into visible vessels in the the liver.
In patients with slow growing large cancer that are not removable by surgery, liver transplant is an option. Patients can have a prior site where the cancer was removed, such as the pancreas. However to be considered a liver transplant, there can be no cancer outside the liver or invasion of cancer into visible vessels in the the liver.
These are non-cancerous benign tumors of the liver. They are also the most common tumors of the liver and occur mostly in people ages 30 - 50. Women are affected more and usually have bigger tumors than men. Most hemangiomas do not produce symptoms. But patient can feel fullness or a pressure type of pain. As hemangiomas increase in size, they can bleed; especially if greater than 10 centimeters in size and peripherally located.


This is usually a non-cancerous benign tumor of the liver. It is associated with use of birth control pills. Most adenomas have no symptoms. However, once an adenoma grows more than 5 centimeters in size, patients can describe a feeling of fullness. In up to 4 out of 10 patients, an adenoma can bleed. Patients can feel pain, loss of appetite, nausea, vomiting, fever, and sometimes shock. In 1 out of 10 patients, the adenoma can turn into a liver cancer. Once an adenoma reaches 5 centimeters in size, it should be removed.
Focal nodular hyperplasia (FNH) is a benign condition of the liver that is often discovered incidentally on radiological exam. FNH has no malignant potential, is rarely symptomatic and surgery is almost never required. FNH occurs most commonly in premenopausal women, but up to 10% of patients are men. Occassionally FNH can cause symptoms such as pressure, fullnes or pain, as well as demonstratng rapid growth. These findings can be indications for surgical removal. Prior to surgery, patients should have a thorough investigation to rule out other causes of symptoms, such as an upper endoscopy.
Liver cysts are thin-walled structures that are filled usually with clear fluid. Most are simple and single in number. Sometimes a cyst will increase in size, causing feeling of fullness, discomfort, or pain. On rare occassions, a patient can bleed into the cyst. This can cause sudden and severe right upper-abdomen and shoulder pain. Simple liver cysts are not associated with cancer. If a patient suffers from discomfort or or pain, the best treatment is to remove a large portion of the cyst wall. This is called a marsupialization, and can usually be done with a laparoscope. This is usually a same day procedure. The risk of the cyst returning is 5-10%.
If the cyst is complex; meaning it has multiple divisions within or uneven wall thickening, a cystic tumor may exist. About 1-2% of cystic tumors contain a cancer. Cystic tumors should be entirely removed surgically. If there is suspicion of a cystic tumor, the cyst fluid should be obtained and sent for testing of tumor markers.
In very rare cases, patients can have clusters of cysts that spread through out the liver. This is called polycystic liver (PLD) disease. Over many years, patients can develop massive liver enlargement, causing abdominal swelling and pain. Although PLD does not cause liver failure, in extreme cases, the patient may needs a liver transplant.
If the cyst is complex; meaning it has multiple divisions within or uneven wall thickening, a cystic tumor may exist. About 1-2% of cystic tumors contain a cancer. Cystic tumors should be entirely removed surgically. If there is suspicion of a cystic tumor, the cyst fluid should be obtained and sent for testing of tumor markers.
In very rare cases, patients can have clusters of cysts that spread through out the liver. This is called polycystic liver (PLD) disease. Over many years, patients can develop massive liver enlargement, causing abdominal swelling and pain. Although PLD does not cause liver failure, in extreme cases, the patient may needs a liver transplant.
Surgical Shunt
Complications of portal hypertension (bleeding and/or ascites)
Gastric devascularization (open and laparoscopic)
Complications of portal hypertension (bleeding)
Complications of portal hypertension (bleeding and/or ascites)
Gastric devascularization (open and laparoscopic)
Complications of portal hypertension (bleeding)